Call us 1800 243 232
Call us 1800 243 232
The spinal cord is:
The spinal cord plays a key role in all our daily activities. It takes nerve signals, or messages, from the brain to the body. These messages command the muscles we use to move.
The spinal cord also receives sensory input (sensations such as touch, temperature and pain) from the body, processes some of this input, and then takes that information to the brain.

The spinal cord also acts independently of the brain for some movements, for example reflexes.

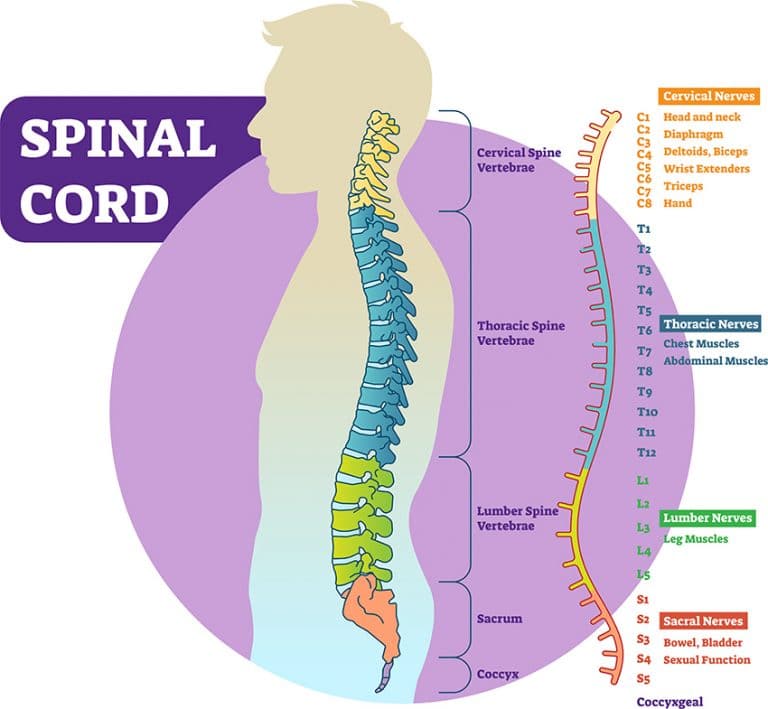
There are 31 pairs of spinal nerves that come from the spinal cord and go out into the body.
The spinal nerves are divided into 5 sections. These sections are named according to where the nerves come out through the vertebrae. Understanding where nerves leave the spinal column and what function the nerves control is important when thinking about spinal trauma.
Click this link to read more about the anatomy of the spinal cord and nerves.
Source: https://www.shelteringarms.com/conditions-and-services/outpatient-services/spinal-cord-injury/
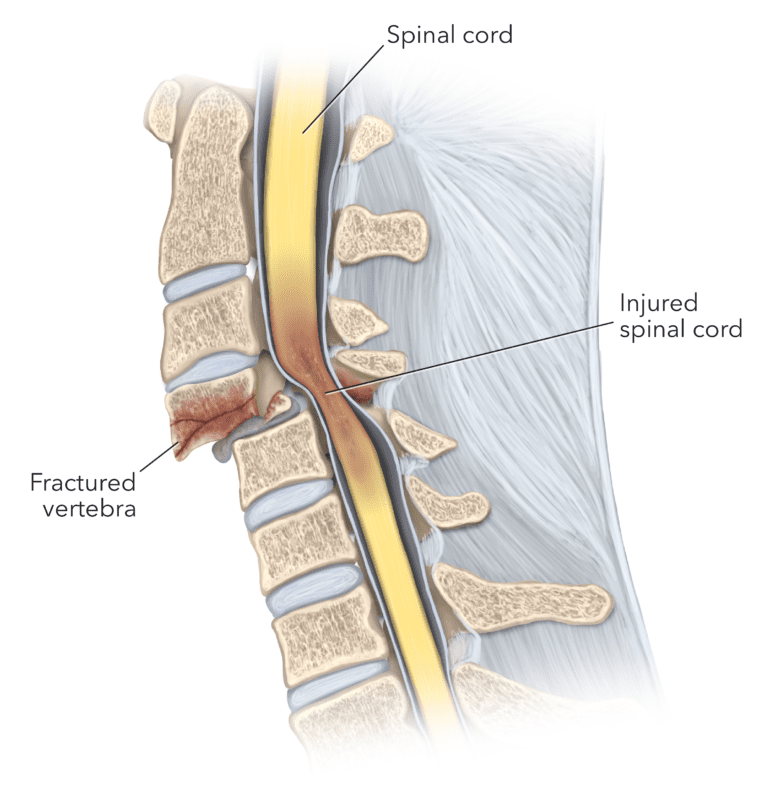
Spinal cord injury occurs when there has been damage to the spinal cord which leads to a loss of function and feeling in the body. Spinal cord injury impacts mobility and movement as well as bodily functions such as breathing, digestion and sexual function.
Spinal cord injury can be caused by a trauma or non-traumatic issues such as arthritis, cancer, inflammation, infections and disease, or disk degeneration. In Australia around 20% of all spinal injury cases are non-traumatic.
Traumatic Spinal Cord Injury (SCI) occurs when an external physical impact (for example, a motor vehicle injury) suddenly damages the spinal cord.
Source: https://drarvindjaga.com/we-treat/neurological-conditions/spinal-cord-injury-treatment-in-jaipur/
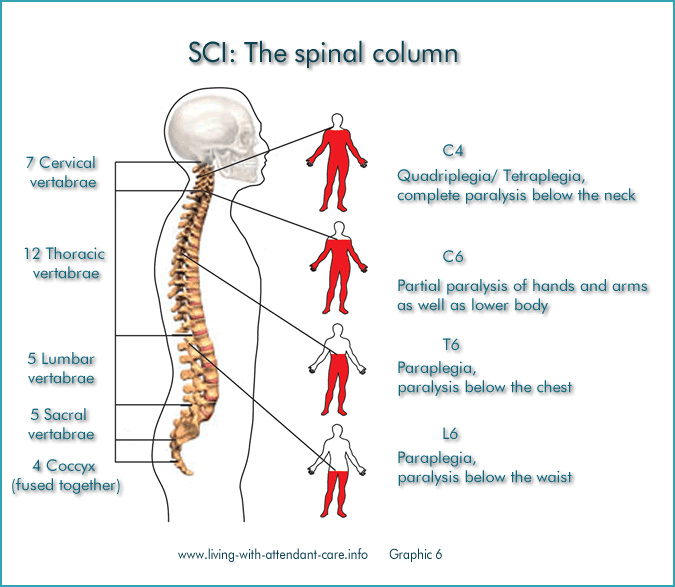
Every person will experience different losses in function and sensation. Some injuries are complete, while others can be incomplete. The spinal cord can be severed or squashed or bruised or a combination of these.
Damage to the spinal cord at the thoracic or lumbar region (the back and lower back) results in paraplegia, where the person can have full use of arms and hands but no control of the lower limbs.
Damage in the cervical region (the neck) results in quadriplegia, also referred to as tetraplegia, where the person loses control of their arms and hands as well as their legs.
Every person will experience different losses in function and sensation. Some injuries are complete, while others can be incomplete. The spinal cord can be severed or squashed or bruised or a combination of these.
Source: http://www.living-with-attendant-care.info/Content/Spinal_Cord_Injury_d_Injury_Effect_Impact.html
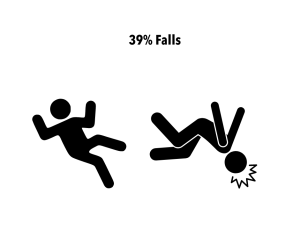
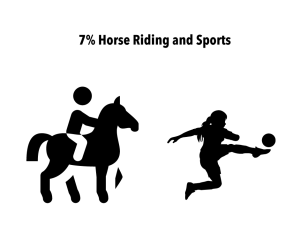
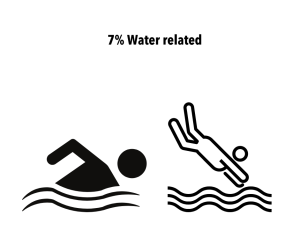
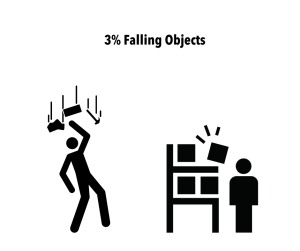
Click to see the % breakdown of traumatic spinal injury causes.
Click to read more
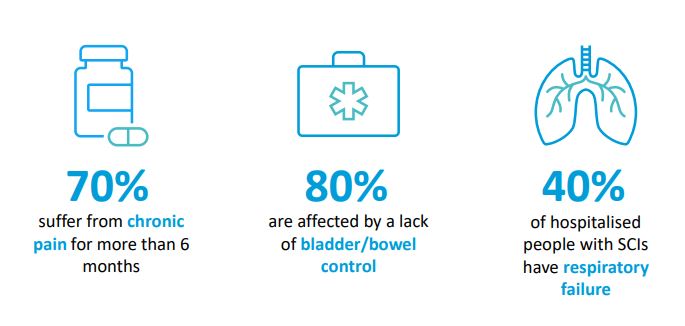
The Australian spinal cord injury survey of Australians living with an SCI found that people rated bladder or bowel control, chronic pain and lack of hand function (for tetraplegic injuries) as the most significant factors impacting their quality of life and would prefer to regain these three functions over all other functions.
There are six critical areas of care that it is important for you to understand when supporting a client living with a spinal cord injury. Some clients may be very aware of these and be active in their care however other clients will need your support to maintain appropriate levels care.
Sudden injuries, such as traumatic SCIs, are likely to impact a person’s mental health and wellbeing. Beyond Blue estimates that up to 40% are likely to suffer PTSD and 30%are at risk of depression.
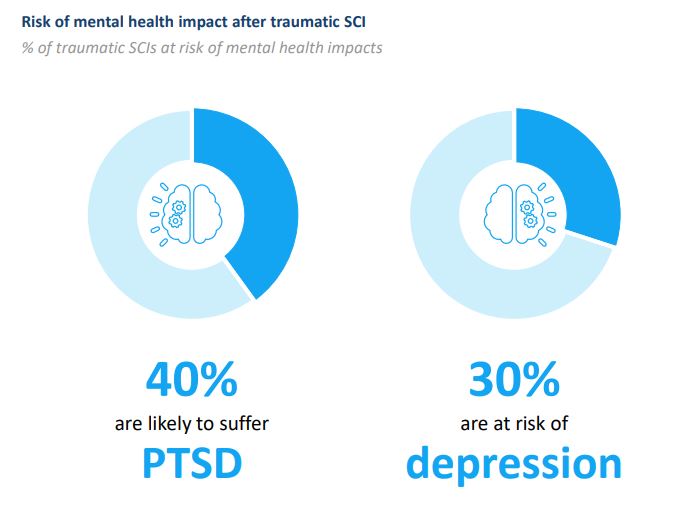
Following a spinal cord injury people can experience increased challenges with their mental health. This might include sleep disturbance and cognitive problems. There may be grief and loss, trauma, pain, financial impact, isolation, additional physical deterioration, and family impacts. Some people will experience depression. All of these are very common and take time and help to overcome.
“Life with a spinal cord injury is challenging but challenges can be rewarding, satisfying and fun. Lean into the discomfort and you will find your way, there are so many opportunities to find beauty and enjoyment.” Person with L1 paraplegia
To read Case Study see page 13 of the report here
After a spinal injury, a client may not have the same control over their bladder. This is called a neurogenic bladder.
Bladder control happens at the sacral nerve level, and it is a reflex responding to the filling of the bladder. If an injury is higher than the sacral area then there should be no problem with this reflex. However, the brain controls the reflex helping a person to hold on and telling you when to empty.
There are two types of neurogenic bladder:
Things to consider: A client may have a permanent catheter or catheterise intermittently, infection is the major concern to monitor for, as well as blocks to the catheter.
The sacral nerves are responsible for bowel movements. There are two types of problems after spinal cord injury and is called a Neurogenic bowel.
Things to consider: The importance of a bowel routine and watch for signs of constipation.
The decreased or lack of sensation and movement increases the risk of skin issues.
The lack of sensation can mean a client will not notice if they bump themselves or cut themselves and they are more at risks of burns from hot and cold items.
Pressure from not moving can cause areas of redness and develop into pressure sores where the skin and tissue under the skin is damaged, breaking down to form an ulcer.
There is a reduced capacity to sweat or shiver causing difficulties with maintaining body temperature.
Things to consider:
It would seem a little ironic that people with a spinal cord injury and little to no sensation can feel pain, but they can, and it is common. Studies suggest that two thirds of people with spinal cord injury experience chronic pain and one third severe pain.
Pain can be experienced above the level of injury, at the level of injury or below the level of injury.
Feeling pain is also linked to a complete or incomplete spinal injury. Sensory loss can vary in an incomplete injury from minimal loss to complete loss.
Different types of pain after spinal cord injury include:
Things to consider: Bladder infection, constipation, fatigue, depression and anxiety and stress can make pain worse. Medications or being distracted or using gentle movement/exercise can reduce pain.
Autonomic dysreflexia (also known as hyperreflexia) is a medical condition that causes a sudden rise in blood pressure in a person with a spinal cord injury, at or above, the T6 spinal level.
It is an important condition to understand as it is considered life threatening.
People with a complete spinal cord injury have a much higher incidence of autonomic dysreflexia: 91% with a complete injury versus 27% with an incomplete injury.
The autonomic nervous system is the part of the nervous system that supplies your internal organs. The autonomic nervous system controls internal body processes such as blood pressure, heart rate, body temperature and digestion. Autonomic dysreflexia is a sudden increase in blood pressure due to a problem below the level of spinal cord injury. The problem causes irritation and overactivity in the part of the nervous system responsible for controlling blood pressure. This is a medical emergency and needs treating, and the cause removed.
Autonomic dysreflexia is most commonly triggered by a cause related to the bladder or bowel.
Bladder causes
Bowel and abdominal causes
Other causes
Thank you for taking part in Anglicare’s Spinal Cord and Traumatic Injury Training. Please complete the short quiz below to finish the training.
|
|