Call us 1800 243 232
Call us 1800 243 232
This session is designed to support you to maintain your health and wellbeing while working with people with a disability, whether in a residential or community setting.
At the end of this module, you will be able to:
This session will take around 10 minutes to complete. At the end, you will be required to complete a short, comprehensive quiz.
This training has been adapted from the Australian Government’s Aged Care Module 5 session. The information in this session is consistent with COVID-19 Guidelines for Outbreaks in Residential Care Facilities.
Information regarding the COVID-19 pandemic is continually evolving, so please ensure that you regularly review the information at the Australian Government Department of Health, as well as the Tasmanian Government Coronavirus website.
You can also find answers to come frequently asked questions about COVID-19 on Confluence here.
PPE is one element of good practices (precautions) that prevent the spread of infection. The precautions are divided into:
These occur routinely in all care settings and encounters with the people we support.
Standard precautions routinely protect staff and people we support from infections disease. They are the minimum infection control standard when in contact with others in care.
They require staff to:
These are all routine requirements when caring for others.
These depend on how the infection is spread (transmitted from one to another). The vast majority of the spread of COVID-19 is believed to occur from large droplets of infection particles produced when coughing.
The cough produces large infection droplets which fall about a metre away from the mouth. This is why we have been asked to stay 1.5 metres away from each other. If someone coughs directly on you within this space you can inhale the particles.
These droplets land on materials close to the ill person and may survive on the surface for a period from hours to 3 days. This is why we have been asked to increase cleaning and sanitizing of the environment around people with COVID-19.
If another person touches the surface they can pick up the infectious virus on their skin. However, they will not be infected unless they pass this particle into their body through their nose, eyes or lips. This is why we have been asked to avoid touching our faces.
So, standing more than 1.5 metres back from an ill person means we are using distance as a barrier and do not need PPE. If you are talking to someone you support from the door to their room you do not need PPE.
If you are within 1.5 metres of a person who is suspected or confirmed to have COVID-19 you need PPE for contact and droplet precautions. This includes a:
Staff working in a Residential Facility must change their PPE and perform hand hygiene after contact with any person they are supporting who is suspected or confirmed to have COVID-19 or when moving from one room to another.
The large particle droplets as described previously account for most of the transmission of COVID-19.
Far less commonly, an ill person will be in a situation, or undergoing a procedure in hospital, that makes small particle aerosols. These small particles are able to float around in the air and can be breathed in by others far away. Measles is spread this way which is why it is so infectious.
A nebuliser is used to transfer medicine into mist for a person to breath in. A nebuliser creates dangerous aerosols. Nebulisers should never be used during the covid-19 outbreak. A spacer that holds inhalant material such as Ventolin is a suitable alternative.
A person who is coughing excessively, might make aerosols.
If a person is coughing excessively:
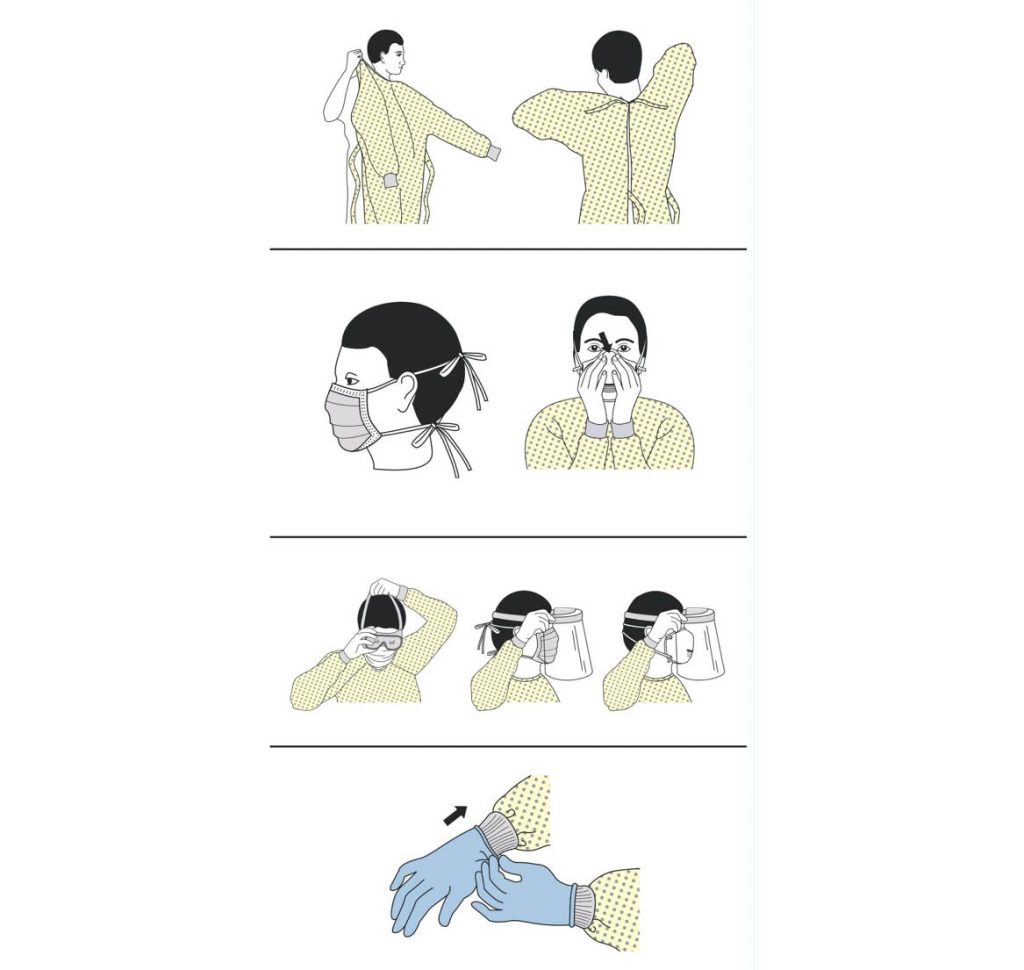
Ensuring that PPE is fitted and removed in the correct order is important because it protects you from accidental contact with viruses and infectious diseases.
Hand hygiene should always be performed before putting on PPE.
The correct order for putting on PPE is:
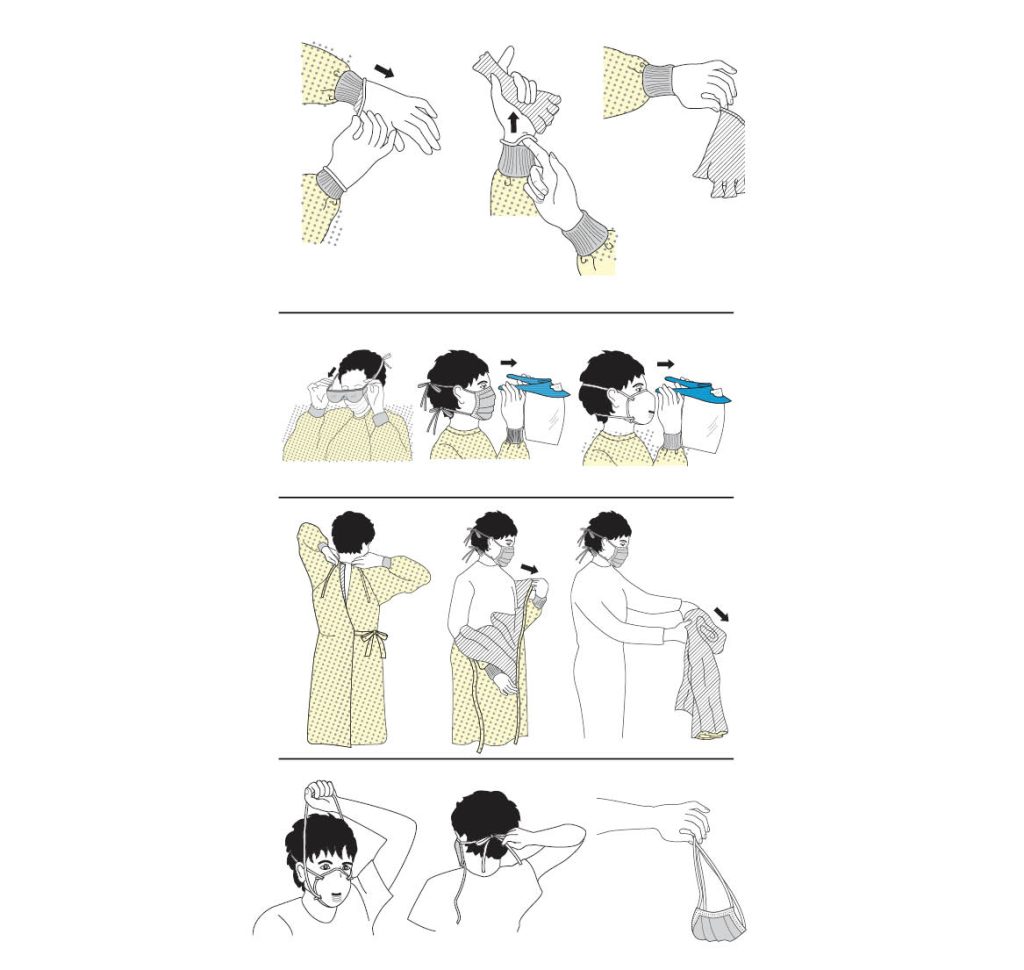
PPE should be removed in a manner that prevents contamination of the staff member’s clothing, hands and environment.
Hand hygiene should be performed after removing and discarding each item of PPE.
The correct order for removing PPE is:
When caring for anyone with suspected or confirmed COVID-19, staff should use droplet transmission-based precautions.
Before Ben enters Edna’s room he should put on a:
After Ben has finished assisting Edna, he should:
Thank you for taking part in Anglicare’s Personal Protective Equipment Training. Please complete the short quiz below to finish the training.